Earache, No Infection (Adult)
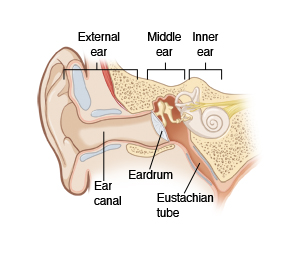
Earaches can happen without an infection. They can occur when air and fluid build up behind the eardrum. They may cause a feeling of fullness and discomfort. They may also impair hearing. This is called otitis media with effusion (OME) or serous otitis media. It means there is fluid in the middle ear. It is not the same as acute otitis media, which is often from an infection.
OME can happen when you have a cold if congestion blocks the passage that drains the middle ear. This passage is called the eustachian tube. OME may also occur with nasal allergies or after a bacterial infection in the middle ear. Other causes are:
-
Trauma.
-
Bacterial infection of the mastoid bone (mastoiditis).
-
Tumor.
-
Changes in pressure, such as from flying or scuba diving.
The pain or discomfort may come and go. You may hear clicking or popping sounds when you chew or swallow. You may feel that your balance is off. Or you may hear ringing in the ear.
It often takes from several weeks up to 3 months for the fluid to clear on its own. Oral pain relievers and ear drops help if there is pain. Decongestants and antihistamines sometimes help. Antibiotics don't help since there is no infection. Your doctor may give you a nasal spray to help reduce swelling in the nose and eustachian tube. This can allow the ear to drain.
If your OME doesn't get better after 3 months, surgery may be used to drain the fluid. A small tube may also be put in the eardrum to help with drainage.
Because the middle ear fluid can become infected, watch for signs of an infection. These may develop later. They may include increased ear pain, fever, or drainage from the ear.
Home care
These home-care tips will help you take care of yourself:
-
You may use over-the-counter medicine as directed by your doctor to control pain, unless medicine was prescribed. Talk with your doctor before using any medicines if you have chronic liver or kidney disease, or ever had a stomach ulcer or GI bleeding. Also talk with your doctor if you take any other medicines, especially blood thinners.
-
Ask your doctor if you may use over-the-counter decongestants, such as phenylephrine or pseudoephedrine. Keep in mind they are not always helpful.
-
Talk with your doctor about using nasal spray decongestants. Don't use them for more than 3 days, or as directed by your doctor. Longer use can make congestion worse. Prescription nasal sprays from your doctor don't often have such restrictions.
-
Antihistamines may help if you are also having allergy symptoms.
Follow-up care
Follow up with your doctor as advised.
When to get medical advice
Contact your doctor right away if you have:
-
Ear pain that gets worse or that does not start to get better.
-
A fever of 100.4°F (38°C) or higher, or as directed by your doctor.
-
Fluid or blood draining from the ear.
-
Headache or sinus pain.
-
Changes in hearing.
Call 911
Call 911 if you have: