Pharyngitis (Sore Throat), Report Pending
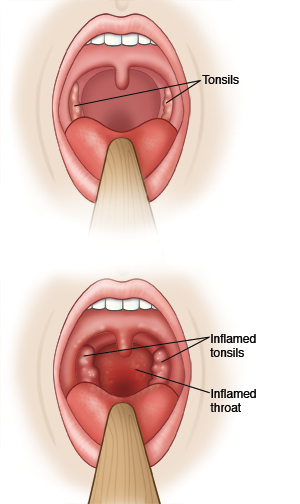
Pharyngitis (sore throat) is often due to a virus. It can also be caused by strep (streptococcus) bacteria. This is often called strep throat. Both viral and strep infections can cause symptoms such as throat pain that is worse when swallowing, aching all over, headache, and fever. Both types of infections are contagious. They may be spread by droplets when an infected person coughs or sneezes. Or they may spread when the droplets get on objects or parts of your skin that come in contact with your mouth, nose, or eyes.
A test has been done to find out if you or your child has strep throat. Often a rapid strep test can be done that gives immediate results and treatment can begin right away. A throat culture may also be done. The culture results take longer. If you have a virus, the culture results will be negative. The facility will call with your culture results. Call this facility or your doctor if you were not given your culture results for strep. If a test is positive for strep infection, you will need to take an antibiotic. An antibiotic is a medicine used to treat a bacterial infection. A prescription will be sent to your pharmacy. Or a written copy will be given to you at that time. If both tests are negative, you likely have a virus, usually viral pharyngitis. This does not need to be treated with antibiotics. Until you receive the results of the rapid strep test or the throat culture, you should stay home from work. If your child is being tested, they should stay home from school.
Home care
-
Rest at home. Drink plenty of fluids so you won't get dehydrated.
-
If the test is positive for strep, you or your child should not go to work or school for the first 24 hours of taking the antibiotics or as directed by the doctor. After this time, you or your child will not likely be contagious. You or your child can then return to work or school when feeling better or as directed by this facility or your doctor.
-
Use the antibiotic medicine (often penicillin or amoxicillin) for the full 10 days or as directed by the doctor. Don't stop the medicine even if you or your child feels better. This is very important to make sure the infection is fully treated. It's also important to prevent medicine-resistant germs from growing. Treatment for 10 days is also the best way to prevent rheumatic fever, which affects the heart and other parts of the body. If you or your child was given an antibiotic shot, the doctor will tell you if additional antibiotics are needed.
-
Adults can use throat lozenges or numbing throat sprays to help reduce pain. Gargling with warm saltwater will also help reduce throat pain. Dissolve 1/2 teaspoon of salt in 1 glass of warm water. First discuss this treatment with your doctor.
-
Children can sip on juice or ice pops. Children 5 years and older can suck on a lollipop or hard candy. Children 6 years and older can try gargling with warm saltwater as well.
-
Don't eat salty or spicy foods or give them to your child. These can irritate the throat.
Other medicine for a child: Give your child acetaminophen or ibuprofen for fever, pain, or fussiness. Do not use ibuprofen if your child is less than 6 months old unless the doctor gave you instructions to use it. Be safe with medicines. Read and follow all instructions on the label. Do not give aspirin to children or teens unless your child's doctor says it is safe. Aspirin can put your child at risk for Reye syndrome, a rare but serious condition.
Other medicine for an adult: Ask your doctor if you can take an over-the-counter pain medicine, such as acetaminophen, ibuprofen, or naproxen. Be safe with medicines. Read and follow all instructions on the label.
Follow-up care
Follow up with the doctor or our staff if you or your child doesn't feel or get better within 72 hours or as directed.
When to get medical advice
Contact the doctor right away if you or your child:
-
Has a fever of 100.4°F (38°C) or higher, or as advised by your doctor (see "How to take a child's temperature" below).
-
Has ear pain, sinus pain, or headache that is new or getting worse.
-
Has painful lumps in the back of neck.
-
Has a stiff or swollen neck.
-
Has lymph nodes that are getting larger or has swelling of the neck.
-
Can’t open the mouth wide due to throat pain.
-
Has signs of dehydration, such as very dark urine, no urine, or sunken eyes.
-
Has noisy breathing.
-
Has a muffled voice.
-
Has a new rash.
-
Has new or worse symptoms.
Call 911
Call 911 if you or your child:
Prevention
Here are steps you can take to help prevent an infection:
-
Keep good hand-washing habits.
-
Don’t have close contact with people who have sore throats, colds, or other upper respiratory infections.
-
Don’t smoke, and stay away from secondhand smoke.
-
Stay up-to-date with all of your vaccines.
How to take a child's temperature
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The doctor may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The doctor may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the doctor what type to use instead. When you talk with any health care provider about your child’s fever, tell them which type you used.